My Thoughts About Science
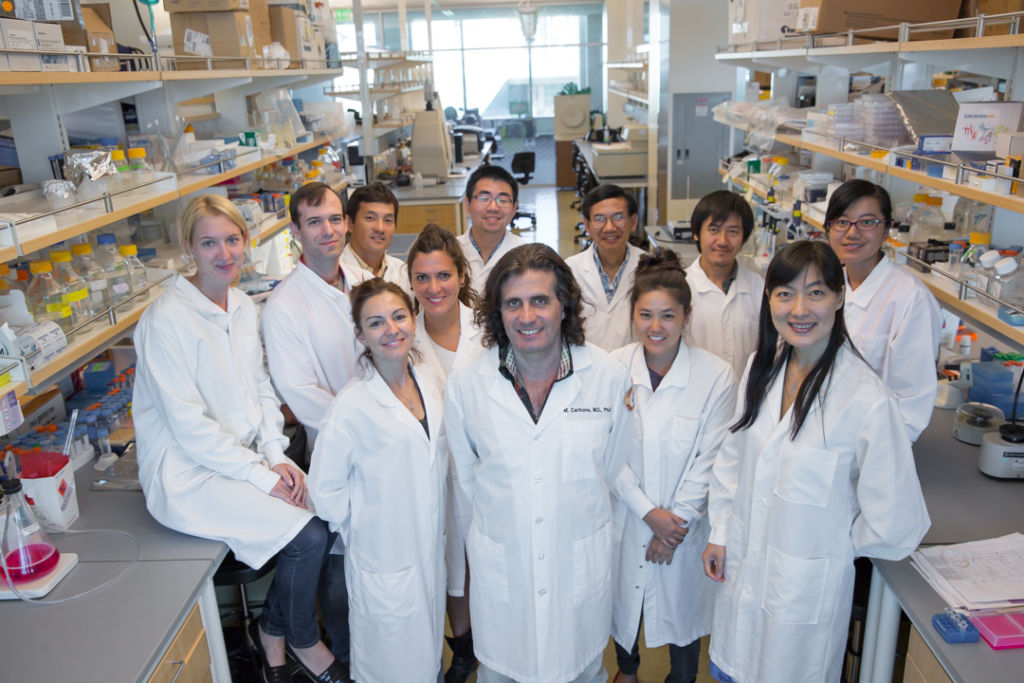
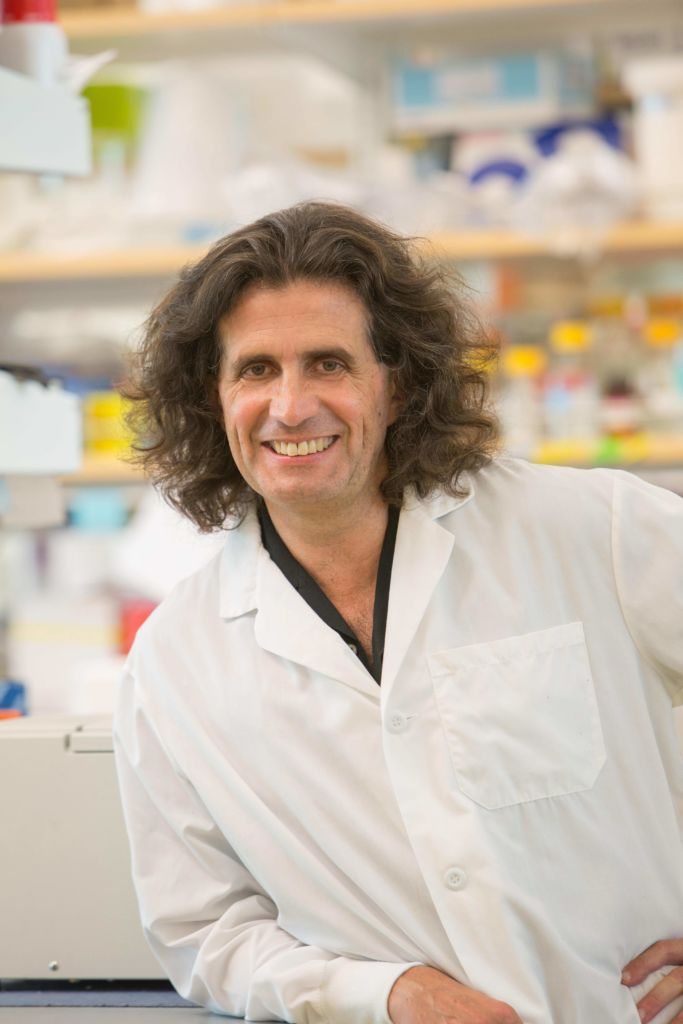
Politicians and Promises – Dr. Michele Carbone
I had to go to Turkey to find–for the first time in my life–politicians who made promises and actually honored them! Dr. Salih Emri, the one with the “Lei”, came to visit us at our laboratory at the University of Hawaii Cancer Center in Honolulu. He was the right hand of Dr. Baris: together we spent many days and nights studying a devastating epidemic of mesothelioma in the Cappadocian villages.
Together over dinner on the Red River we convinced Baris to come with us and with Umran Dogan our mineralogist, to meet the Turkish Ministry of Health to try to convince him to build new villages free of erionite and transfer there the whole population to prevent mesothelioma in future generations. It seemed an “impossible” dream. Yet, against all odds we succeeded: 2 new villages were built and the entire population of Tuzkoy and Karain moved to safe homes. Of course that was thanks to the Ministry of Health and also to Dr. Murat Tuncer, then Director of Cancer Control and later Rector at University of Hacettepe, who became passionate with the project and worked hard to ensure that the villagers rapidly had new safe homes, and -thanks to Murat- even a small clinic was built in Tuzkoy. I had never seen politicians and executives work so hard to help their own people, getting no personal reward for that.
Link to LinkedIn post from Dr. Michele Carbone, MD, PhD on May 26, 2018

Surgeon or pathologist?
Do you know that I wanted to be a plastic surgeon?
I did my thesis in plastic surgery, was accepted in a residency in plastic surgery, and then, as I worked for a few months with a plastic surgeon, I decided that was not for me and I decided instead to accept a residency in pathology, to the great disappointment of my father who was an orthopedic surgeon and who I think did not consider anybody a real “doctor” unless they were surgeons!
So how did that happen?
Well, I found myself enjoying studying more about the biological process that caused diseases, reading about those people who had made fundamental discoveries that had improved the human condition, than learning surgery. Many people told me I was nuts to turn down a residency in plastic surgery: In fact I never regretted it. I do not think I would have been a good plastic surgeon, to be good at something you must love what you do: I did not love doing surgery.
Instead with a little bit of luck and together with my fantastic team, we are developing new preventive and therapeutic approaches that we will soon test in clinical trials and that I hope will fix for good this terrible cancer we study called mesothelioma.
Link to LinkedIn post from Dr. Michele Carbone, MD, PhD in May 2018
Obesity and cancer
In 2014, about 630,000 people in the U.S. were diagnosed with overweight- or obesity-linked cancer.
Next to smoking, maintaining a healthy body weight is the most important thing people can do to lower their risk of cancer. The American Institute for Cancer Research h
as stated that in the U.S., maintaining a healthy body weight can prevent the following cancers:
- 22% of gallbladder cancers
- 11% of advanced prostate cancers
- 5% of ovarian cancers
- 33% of esophageal cancers
- 19% of pancreatic cancers
- Around 24% of kidney cancers
The American Institute for Cancer Research also stated that maintaining both a healthy body weight and being active can prevent the following:
- 50% of colorectal cancers
- 33% of breast cancers
- 30% of liver cancers
- 59% of endometrial cancers and more!
So what should we do to fight this problem and help people not get sick? The article writes the usual obvious logical things that you can be sure tht people who are obese will not do: “Avoid high-calorie food and sugary drinks” and so on!. I think it would be more effective and practical to simply send the medical bills of taking care of obese patients to fast food companies!: they would disappear and most people would be fit again!

After 20 years scientists figured out why BRCA1 mutations cause cancer:
Zhao et al Nature October 4
Our team discovered and named the BAP1 cancer syndrome (Testa JR et al., Nature Genetics 2011, Carbone et al., Nat Rev Cancer 2013) and it is both intriguing and exciting to see commonalities between how BRCA1 and BAP1 work. Zhao et al discovered that the BRCA1-BARD1 complex is indispensable for RAD51 stimulation in DNA repair by homologous recombination. Similarly, El Bachir Affar’s team discovered that BAP1 regulates homologous recombination (Yu H et al., PNAS 2014). In addition, we discovered that BAP1 regulates cell death by deubiquitylinating and stabilizing the IP3R3 receptor and thus regulating calcium fluxes inside the cell (Bononi et al., Nature 2017) . Since calcium is also required for the Krebs cycle, BAP1 mutations impair aerobic respiration forcing cells carrying BAP1 mutations into aerobic glycolysis (Warburg effect) (Bononi et al., Cell Death Differentiation 2017). These additional activities of BAP1, account for the much more powerful tumor suppressor activity of BAP1: 100% of carriers of germline mutations have develop one or more malignancies in their lifetime (Baumann F et al., Carcinogenesis 2015) compared to BRCA1.
A very good example of why it is important to fund cancer research. Brain gliomas are among the most lethal cancers: they cannot be excised surgically and they are resistant to all available therapies. Ted Kennedy died of this cancer and John McCain is dealing with this problem now. An exciting discovery reported by Venkatesh et al in the Sept 28, 2017 issue of Nature provides a novel target that may well change this dismal prognosis.
Targeting neuronal activity-regulated neuroligin-3 dependency in high-grade glioma
Glioma growth requires a cleavage product of Nlgn3 a protein secreted by non malignant neurons in the microenvironment (David AM et al., Nature 1990). Vankatesh et al, demonstrated that human glioma cells do not grow when transplanted into brain of Nlgn knockout mice (i.e., mice that cannot produce Nlgn3). Moreover, they identified Adam 10 as the protease that cleaves Nlgn3 and demonstrated that treatment with small molecule inhibitors of Adam 10 impaired human glioma growth transplanted into the brain of mice. Finally we have a specific target to develop effective therapies for this devastating malignancy

25 MAY 2017 | VOL 545 | NATURE | 387 – Publish Houses Made of Brick, Not Mansions Made of Straw: I read this editorial by W. Kaelin. He notes that presently papers in major journals contain an overwhelming amount of data that even reviewers have hard time to follow. In fact, presently the main figures represent only a small fraction of the data, the majority of the data are published as supplementary data. A paper in Nature has 4 figures, each with about 10 panels, plus 10 supplementary figures each formed by about 10 panels. Each panel is usually its own figure, so we have a total of ~140 figures, each with its own standard deviation (minimum of 3 experiments), which totals to ~420 experiments. Plus Tables. This when I grew up was called a book! Not only the cost of producing a paper of this size are prohibitive to many, but almost nobody will ever read the supplementary data, maybe the reviewers. So why are we doing this? Look we are doing this to ourselves because are the reviewers who ask for this huge amount of data, not the editors. Last year at a Weinman Symposium I asked Randy Shekman (Nobel Prize winner 2013) if he thought the quality of science had improved as a result of the amount of data presently required to publish in top journals: “Of course not” was his answer. So why are we doing this to ourselves?
Tomatoes taste great and are also healthy. I look always with lots of skepticism at the myriad of epidemiological papers claiming that eating this or that food prevents cancer and/or makes you live longer. The list is infinite because there is nothing easier to write than that: there will always be some statistical formula that will allow someone to claim that this or that food keeps you healthy. This pseudo-science sells well on the news and it is cheap to produce -of course there are exceptions as there are well controlled epidemiological papers on the relationship between the intake of certain foods and cancer, but they are rare. With this premise, I found unusually interesting the paper by Daniela Barone et al. DOI: 10.1002/jcp.25995, which I read because it is from the lab of a respected researcher, Dr. A. Giordano. The Authors analyzed in vitro the lipophilic extracts of two variants of Italian tomatoes and found that they inhibited growth and invasion of 3 different gastric cancer cell lines apparently by inducing RB and RB-related protein activities. The study seems well controlled. These data bring some mechanistic evidence into the well accepted notion that a Mediterranean diet is healthy.

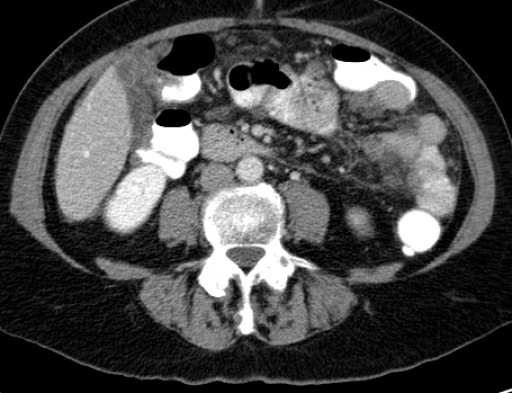
Many of us are seeing an increasing number of cases of peritoneal mesothelioma in young people with no evidence of exposure to asbestos or erionite. In April of this year we published in JAMA Oncology about an epidemic of peritoneal mesothelioma in young women in China:
Association of Asbestos Exposure With Malignant Mesothelioma Incidence in Eastern China
In the current issue (Sept 14) of JAMA Oncology (doi:10.1001/jamaoncol.2017.2918) Lucian Chirieach’s team at Harvard reported a rearrangement of the ALK gene in 3/88 women with peritoneal mesothelioma not exposed to asbestos. Two of these women were younger than 40. This study extends previous findings reporting an ALK rearrangement in a 10 year old girl with peritoneal mesothelioma, DOI:10.1111/his.12779. ALK rearrangements have been causally linked to lymphomas, carcinomas, etc. Although only a few mesothelioma patients have this genetic alteration, it is important to identify them as personalized ALK- therapy with drugs that target the altered Alk protein, such as Crizotinib, Ceritinib, can help them. As more genetic alterations linked to mesothelioma are identified, and as we develop, or already have, drugs to treat these alterations, more patients will be treated with specific therapies and we will finally make a real impact and improve prognosis, and hopefully save their lives.
The FDA put more Immunotherapy trials on hold as scientists and physicians are starting to they take a much more critical look at benefits versus harm of these trials. https://lnkd.in/gWTXe-D A year ago at the annual IASLC world lung cancer meeting I organized a debate among those who supported checkpoint inhibitors trials in mesothelioma, and those (few) who argued the data were not there yet. It was difficult to find anyone willing to represent the skeptical side: Luciano Mutti, a Professor at University of Salford, Manchester, UK, and one of the leading European physicians treating mesothelioma patients agreed to take the skeptical side and he made a series of very reasonable arguments underscoring for example the low level of genetic mutations found in mesothelioma, the lack of PD-1 expression on most tumor cells, some deaths in phase 1 clinical trials, and argued that we had to develop more data and understand better the mechanisms and what caused harmful side effects before pushing mesothelioma and other cancer patients into immunotherapy trials. It appears that he might have been correct.
FDA Puts Hold on Immunotherapy Trials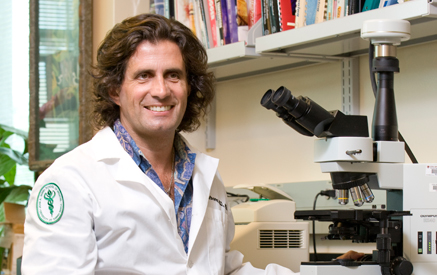
The recent hype of cancer immunotherapy has been phenomenal. It worked so well for melanoma, it will work for everything- Really why? Would you give etoposide to every cancer patient? Patients seem to think that this is the only hope they have to survive cancer, pressure to enter clinical trials is strong. Pharma pushes and doctors go along, editors welcome papers on what is fashionable. Below are the inevitable consequences of rushing new therapies to patients to follow “fashion” rather than scientific evidence and critical analyses of the data. The downside is that not only some patients may not benefit or even suffer harm, but the whole field gets depressed and moves on something else-possibly missing opportunities where Immunotherapy might really help. Like a circus moves from one city to the next we tend to jump from one miracle drug to the next, or one combo to the next, with little critical thinking and apparently not learning from past failures.
Genetics plays a major role in many malignancies.
In a Nature article, Aug 1, doi:10:1038/nature23306, mostly about genetic alterations in metastatic cancers, there is ALSO compelling evidence that genetics plays a much bigger role in cancer than generally accepted. Robinson et al. found that 12.2% of 500 patients with metastatic cancers of different types, developed in individuals carrying germline mutations. 3/4 of mutations were in genes involved in DNA repair! The odds of germline mutations in individuals with metastatic cancers exceeded those found in the population (odds ratio =3.00)! Whether this association is related to the metastatic cancer phenotype studied or whether it is also found in non metastatic cancers was not addressed. Betti M doi: 10.1016/j.canlet.2017.06.028, reported July 4 that 9.7% of mesothelioma patients carry germline mutations of genes involved in DNA repair mechanisms!
These papers reveal that there is a pool of individuals that carry germline mutations that are much more susceptible to cancer, than others. Genetic screening of the population, like the one offered to Nevada residents, will identify individuals with germline mutations and should allow implementation of preventive programs that will save lives.
Link to LinkedIn post from Dr. Michele Carbone, MD, PhD on August 27, 2017

James Brugarola’s team at The University of Texas Southwestern Medical Center at Dallas, reports In the August issue of Cancer Discovery, DOI: DOI: 10.1158/2159-8290.CD-17-0292, that VHL and BAP1 mutations give rise to aggressive renal cell carcinomas clear cell type, while VHL and PBRM1 mutations induce low grade carcinomas.
The same Authors had previously discovered that BAP1 and PBRM1 mutations are mutually exclusive in RCCs. These mice tumors resembled histologically the human tumors and allowed the Authors to discover that they originate from the cells that line the Bowman’s capsule.
The experimental model developed by Dr. Brugarolas is ideal to study renal cell carcinoma, in particular the biological reasons that drive the different tumor behavior in different patients, andto develop specific therapeutic approaches. What remains a mystery is why somatic BAP1 mutations cause an aggressive tumor phenotype in apparently all tumors EXCEPT mesothelioma, and WHY tumors that develop in carriers of germline BAP1 mutations, instead, are usually much less aggressive! and associated with survivals of 5-10 or more years: Baumann F et al Carcinogenesis 2015 doi:10.1093/carcin/bgu227
Link to LinkedIn post from Dr. Michele Carbone, MD, PhD on August 31, 2017

Kornfeld and Titus correctly point that 5 reports of the NAS over 28 years asking for more research to find out why researchers cheat, are misguided because won’t crack misconduct. Then they suggest their own “beautiful” but totally impractical set of remedies. Look, scientists publish inaccurate and fake data to go ahead, as simple as that. Unless we remove this incentive, there will always be those who cheat -like in any work force. In science is easy to fix: limit the biosketch for awarding grants and promotion to the 5 best publications. That will eliminate the urge to publish BS and will allow reviewers the time to actually read the publications, -nobody has the time to read 100+ papers seen in many CVs. This will also increase the chance that fake data will be detected, thus further deterring fakes and sloppiness. It is the concept of quality vs quantity. And if someone argues that for her/him 5 papers are not enough, because she/him is too successful refer her/him to the first line of this article.
Link to LinkedIn post from Dr. Michele Carbone, MD, PhD on August 20, 2017
Cooking really good healthy food.
For those of you who do not know it, I love to cook, and I cook almost every night, for myself or for 100people- not a joke. Since I am “busy” my recipes are simple, fast to make, and of course the best in the world because I like to eat well. Differently than those that you find on the web, I actually prepared these dishes many times myself, so what I write is from experience not hearsay or copied from someone else, who had copied from someone else, and so on and therefore those recipes will never work well because there are too many mistakes. Also I like to be in shape, so my recipes are not going to make you fat! In short, if you want to eat well, go and subscribe to my cooking blog/website -it is free- and you will receive alerts every time I post a new recipe. And of course your feedback is most welcome.
Link to LinkedIn post from Dr. Michele Carbone, MD, PhD on August 6, 2017

Nature editorial: what is wrong in today’s world of science.
Michele Pagano, one of the scientists I admire the most, wrote a beautiful editorial in today’s issue of Nature about the main problem we face in science: quantity versus quality. Which means we are wasting millions to support a lot of inconsequential science rather than focusing our resources to support science that makes a difference. It is a huge yet easy problem to fix it: for cancer research it just needs a stroke of a pen from the NCI director and all the nonsense of BS “science” would be gone in a day: rather than rewarding number of publications, amount of grant funding, etc., reward quality: how did your science help advance our understanding of basic fundamental biological/biomedical problems and/or impact of the science to the life of people. We are cancer researchers to prevent and to find new therapies for cancer, not to accumulate “me too” type publications and money. Anyway read his editorial, is very well written and right to the point. Unless and until we fix the problem Michele discusses, it is and it will be, very difficult to cure cancer because we will never have have enough resources to do so: too much money is wasted to support “me too” type of science or worst.
Link to LinkedIn post from Dr. Michele Carbone, MD, PhD on August 6, 2017

What irrelevant papers mean for science at large
Science is about quality not quantity. This is why the most prestigious journals have a strict peer review system and publish the few papers that survive this rigorous process. These are high impact factor (IF) journals. “Your manuscript has been judged scientifically suitable for publication”. As reviewer, I had rejected it; when the Editor insisted, I wrote: “Very modest contribution”, yet the paper was accepted. This was not one of the “predatory journals” that pop out daily offering to publish anything for a fee. This was one of the mega journals that state “For journals which are not as selective we can now publish as much research as the community wants to read at a lower cost ”. A nice way to say that they publish inconsequential science for a fee! Over 20,000 papers/year: almost nobody reads them. The only reason these journals exist is to make money and support their other “selective” journals. But they corrupt scientists into taking shortcuts and publish inconsequential papers to advance their career; by association they damage us all. How to stop this BS? The despised IF may be our only defense: ignoring biosketches, CVs & grants supported by low IF papers will remove incentives to publish fried air.
Link to LinkedIn post from Dr. Michele Carbone, MD, PhD on August 6, 2017

This is America
Some ~ 20 years ago I took a taxi at Chicago airport to go home. The driver was from Africa, he asks me what do you do? I am doing a residency in pathology at the University of Chicago. He says “I was a Doctor in my country.” I say; why don’t you take the USMLE and get a medical license here? He says: I have no time I have to work to eat. I say: bullshit, I did it, you can do it too, if you want to study you can, don’t you wait hours to get a client at O’Hare? As you wait, study. He says: I have no money to buy the books. I say, look, this is America, stop feeling sorry for yourself and get your medical license, I will give you my books, but only a little bit at the time, you show me you pass USMLE1 and I will give you the books for USMLE2 and 3. He says “OK”. I gave him the books. He came every now and then to my home in Hyde Park to exchange books and to talk. Last time I saw him was 7:00 am: he was really happy, he returned the last set of books, he had passed USMLE3 and got into a residency. I do not know what happened to him, he is practicing somewhere. This is America.
Link to LinkedIn post from Dr. Michele Carbone, MD, PhD on May 29, 2017

Fewer young scientists apply for US grants, WHY?
The American Cancer Society (ACS) sent an email to its members asking why there is a steep drop in grant applications. The ACS funds only investigators in the early stages of their career. So, the number of bright young scientists competing for grants is decreasing. Why? Why wouldn’t? We pay our post docs (i.e., PhDs) ~$47,500, per NIH guidelines. The same PhD can make >100K in a company. That is just the beginning! Then that “crazy” kid who was so in love with science to enter Academia will face a very low grant pay-line –this will likely get worse given the proposed ~20% NIH budget cut. Without a grant he/she has no future in Academia. In this economy good start up packages for young scientists are rare, for a tenure track position you need a grant. When you get a grant, you will be asked to get a second one to cover ~50% of your salary (not easy), or your salary will be reduced. Presently a bright young PhD must love science very much, and needs to be a little bit crazy, to chose Academia. If you do, you better learn quickly how to fund raise and not be dependent exclusively on federal grants that, alone, can no longer support the increasing costs of biomedical research.
Link to LinkedIn post from Dr. Michele Carbone, MD, PhD on May 24, 2017

How we measure scientists, and how we should measure scientists.
I met someone at a meeting. I ask what do you do? “All you need to know about me is that I published 12 papers in the New England Journal of Medicine”. Wow! Am I supposed to be impressed? How do I know if any of those papers turned out to be of some use? Most papers even in top journals are inconsequential. Was this his own research or he only made some minor contribution and got co-authorship? How do I know that? This is the problem in generating artificial “standards” to try to measure scientists and physician. Take the H-index, the most used metrics to compare us. Sure has some value, but will not distinguish between someone who played a minor role, say author 22 out of 40, versus first or senior authors. All authors get the same credit with the H-index, which is nonsense. Moreover, scientists in a large research field obviously get more references than those working on rare diseases. Yet more and more we are evaluated with these unreliable metrics. Much more reliable is to explain in a few sentences how your work has changed our understanding of biology and medicine and/or improved the human condition, how many lives you have saved, and list 1-10 papers to support that.
Link to LinkedIn post from Dr. Michele Carbone, MD, PhD on May 7, 2017

Ethical Dilemma in Research
And what if a person shows up in my office and tells me: I am dying and you could have saved my life with a phone call?
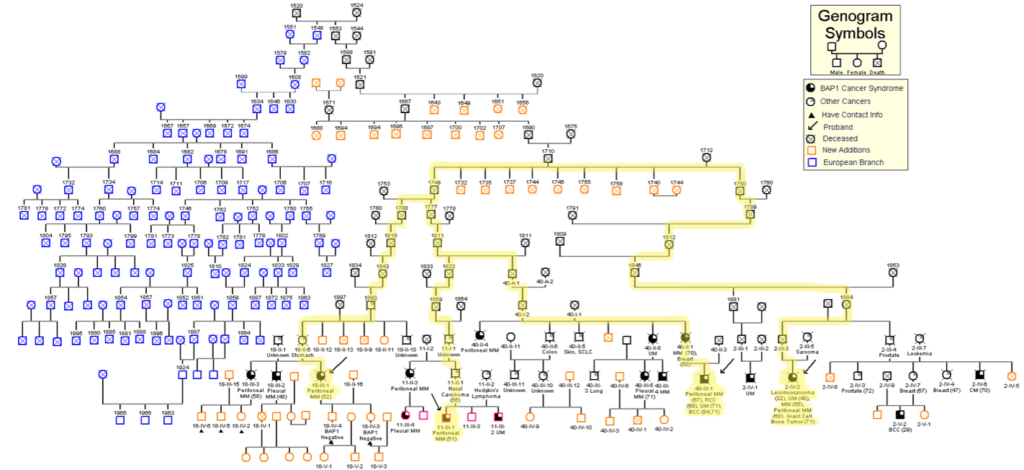
In 2011 we discovered a new cancer syndrome caused by inherited germline mutation of the BAP1 gene (click here for a link to the 2011 article in Nature Genetics). Later, combining genetic, genealogical and molecular studies we connected several families across the world that we found descended from the same couple that immigrated in the US in the early 1700s (Carbone M et al., PLOS Genetics 2015). Using this novel approach we continue to find new branches of these families that are almost certainly obligated mutation carriers. All BAP1 mutation carriers have developed one or more cancers: some are curable ONLY when detected early, i.e., skin and eye melanoma, renal cell carcinoma, etc. So don’t you think we should inform those who are likely mutation carriers, tell them to get tested, so if they do carry BAP1 mutations they can undergo regular medical screening for early detection and curative resection? The IRB, the “ethical committee”, says that it would be intrusion of privacy to call people out of the blue and tell them to get tested. But if we do not call them, they may die and we could have saved them. What are we supposed to do?
Link to LinkedIn post from Dr. Michele Carbone, MD, PhD on April 28, 2017
Why become a doctor?
Why do you want to become a physician?
I used to volunteer in a program that organized meetings between physicians and high-school kids who where considering becoming MDs. The kids answer to my question was invariably “to help people who suffer” or close to that.
Yet when you sit at a table with physicians they usually talk about career, money, the nonsense of administrative issues we have to deal with, or if they are in Academia, they talk about prestigious publications. It is very rare, although fortunately does happen, that the discussion revolves around “what are we doing or what can we do to help people who suffer”. If then you switch the discussion to how your work is evaluated by the Hospital or University administration, the question “what have you done to help patients or people from becoming patients” is rarely on the table: it is all, or almost all, about “how much money you bring into our Institution? And what can we do so that you can bring in more money?”
So either we lied when we were in high school, or something happened along our life and our priorities changed, or we are wasting our life prioritizing issues that are not the reason we became doctors in the first place.
I still try to help people and I measure people based on that.
Link to LinkedIn post from Dr. Michele Carbone, MD, PhD on April 19, 2017

Proposals to restrict H-1B Visas and cut the NIH Fogarty Center will reduce the number of foreign scientists and cause harm to the US and the world. Why wreck a win-win deal?
The best young foreign scientists come to the US to receive advanced training and contribute to technological progress. The US gets some of the best scientists at no cost to us, their education was paid by foreign countries. We select the top 1% of them and offer them permanent residency for “National Interest” –which most take. After 5 years the others go home as required by their Visas, bringing back advanced knowledge gained in the US. They are our ambassadors and help expand local science and create bridges with the US. Foreign scientists help keep the US at the forefront of biomedical research, develop new therapies, and produce patents to keep our economy strong. A post-doc makes ~$46,500/year in Academia: the size of our NIH grants does not allow us to pay more. The same individual makes >$100K if she/he works for the industry. Most US graduates choose Industry. US Academic biomedical research relies on top foreign scientists who are willing to work for less pay: no surprise that they comprise ~25% of the US NAS members.
Link to LinkedIn post from Dr. Michele Carbone, MD, PhD on April 7, 2017
Fake Data in Medical Research
Why do people publish fake data? First let’s distinguish between honest error and deliberate fake. The first is inherent to the human condition. The latter comes in two ways: data that are entirely false, very rare; and data that contain some deliberate manipulation, usually loading controls of protein gels that have been switched, re-used, or Photoshop editing to make the image look better than it is. If one Figure is wrong how can you trust the others? Science self-corrects itself: if others reproduce the data, even if a figure was wrong, the message may be correct. This is usually the case. Then, why would a researcher be so stupid to manipulate an image of an overall correct paper and jeopardize everything? I cannot explain that, but reviewers and editors bear some responsibility when they seem to think that the higher the IF of a journal the more difficult they have to make the life for scientists by demanding “perfect” images rather than focusing on the data’s relevance. This pressure may drive a frustrated student or post-doc, rarely a PI, to use “make up”-very difficult to catch – to improve an image and get the paper published. Perfection is not reality: let us focus on substance.
Link to LinkedIn post from Dr. Michele Carbone, MD, PhD on March 22, 2017

Science in the Era of Budget Cuts to the National Institutes of Health
Next year’s US budget includes a proposed19% cut to the National Institutes of Health (NIH). Even without this cut it is time to look for new ways to fund medical research. In 2002 my modular R01 grant from the NIH was 250K/year. In 2002 Fetal Bovine Serum (FBS) to grow cells in culture was $90/bottle. Today my R01 is 229K/year: the list price for the same bottle of FBS is $750! The cost of all reagents increased, the salary of lab personnel almost doubled. 15 years ago, we could publish a paper in a top journal with ~4 Figures, each with 4 panels. Today reviewers ask for many more (at times unnecessary) supplementary data that few will ever look at. A paper in a top journal often has over 100 panels: each representing multiple experiments –in order to show standard deviation- at the cost of thousand of dollars per panel. How are we supposed to pay for all that? Collaborations and team work helps spread costs. More is needed. A strength of the US is that when the public sector falls short the private sector kicks in: in the future successful labs will need to win grants and ALSO fund-raise via philanthropy, industry, etc.
The era when competitive research can be done only with Federal grants is probably over.
Link to LinkedIn post from Dr. Michele Carbone, MD, PhD on March 16, 2017

The Despised Impact Factor (IF)
Researchers can publish anything we want in a so-called peer reviewed journal: every day, a new journal pops out. Some are legitimate, some are businesses that will publish research for a few thousand dollars. So the fact that a paper was published does not mean it is any good.
Today, I rejected a manuscript that I reviewed for a top journal. The paper was flawed. When I read the Title and Abstract, I did not realize it was flawed. Only when I read the Methods and Result did it become obvious: The research design and approach could not prove what the Authors wanted to prove.
You can bet that paper will end up in a low impact factor (IF) journal. Well, most of the time, we scientists are tempted to read only the Title and Abstract of a peer-reviewed paper! Only when the paper is relevant do we read the full text–and almost never the Methods and Supplementary information. There are not enough hours in a day, and there are too many interesting papers!
So we must rely on others to decide if the research is sound: editors and reviewers. The higher the (despised) IF of a journal, the stricter the review process usually is: thus, the IF, a tool invented by librarians to choose what magazines to purchase, has become the tool we use to decide whether we can trust the conclusions of a paper we have no time to read, and to judge people’s CVs.
Link to LinkedIn post from Dr. Michele Carbone, MD, PhD, posted March 9, 2017.

Is Scientific Research a Passion or a Business?
Surprisingly to me, thousands of people read my brief LinkedIn post on grants. Yet what I wrote everybody in medical research knows. We are measured by grants. If you want a job, if you want to get promoted, the single most important question is “How well are you funded?” Yet grants should merely be tools to make discoveries and save lives from cancer or other diseases. The risk is that while we should be doing something for passion, to better the world, it becomes a business like many others: get money. Fortunately, Nobel prizes, the Lasker Award, and other important prizes are still awarded based on what you have contributed to science and medicine rather than how much money you got for something (and what if you did not do anything good with that money?). A great friend of mine, Dr. Izzettin Y. Baris did a lot of good to this world, and helped save many lives to cancer. He never got a grant! I wrote about him when he died. You can find the story of Baris on my Website, it would be great if young scientists and physicians would take him as an example
Link to LinkedIn post from Dr. Michele Carbone, MD, PhD, posted March 6, 2017.

Chasing Grants
Cancer Research is about finding new ways to prevent or treat cancer, I think. However, we spend a tremendous amount of time chasing grants. We need grants to do the experiments, to do field work, and to pay salaries. But the system has become so much grant-oriented that we are often measured by our peers and Institution by the amount of grants we win rather than the impact of the discoveries we made and the lives we saved to cancer in our research career . When we retire what are we going to answer if someone asks us what did you do to fight cancer? I won 100 grants? And so what? I see many researchers chasing grants rather than innovative ideas: that is the opposite I do. I go, after my ideas, and I never worry about doing a certain research to win a grant. Instead I did my research career by going around the world, looking for new things to study and when I found something that interested me, I tried to make new discoveries and fix the problem: then the grants -I hope- will follow. So far, it has worked quite well!
Link to LinkedIn post from Dr. Michele Carbone, MD, PhD, posted March 3, 2017.